7 Common Myths about Medication-Assisted Treatment
Medication-assisted treatment (MAT) is one of the most effective treatment methods we have in the fight against opioid use disorder (OUD). But despite years of research and patient success stories, it’s still surrounded by stigma and misconceptions. Whether you’re someone exploring treatment options, a loved one trying to help, or a community partner looking to learn more, it’s important to separate myth from fact.
In this blog, we’ll break down some of the most common myths about MAT and share what the evidence really says.
Understanding Medication-Assisted Treatment
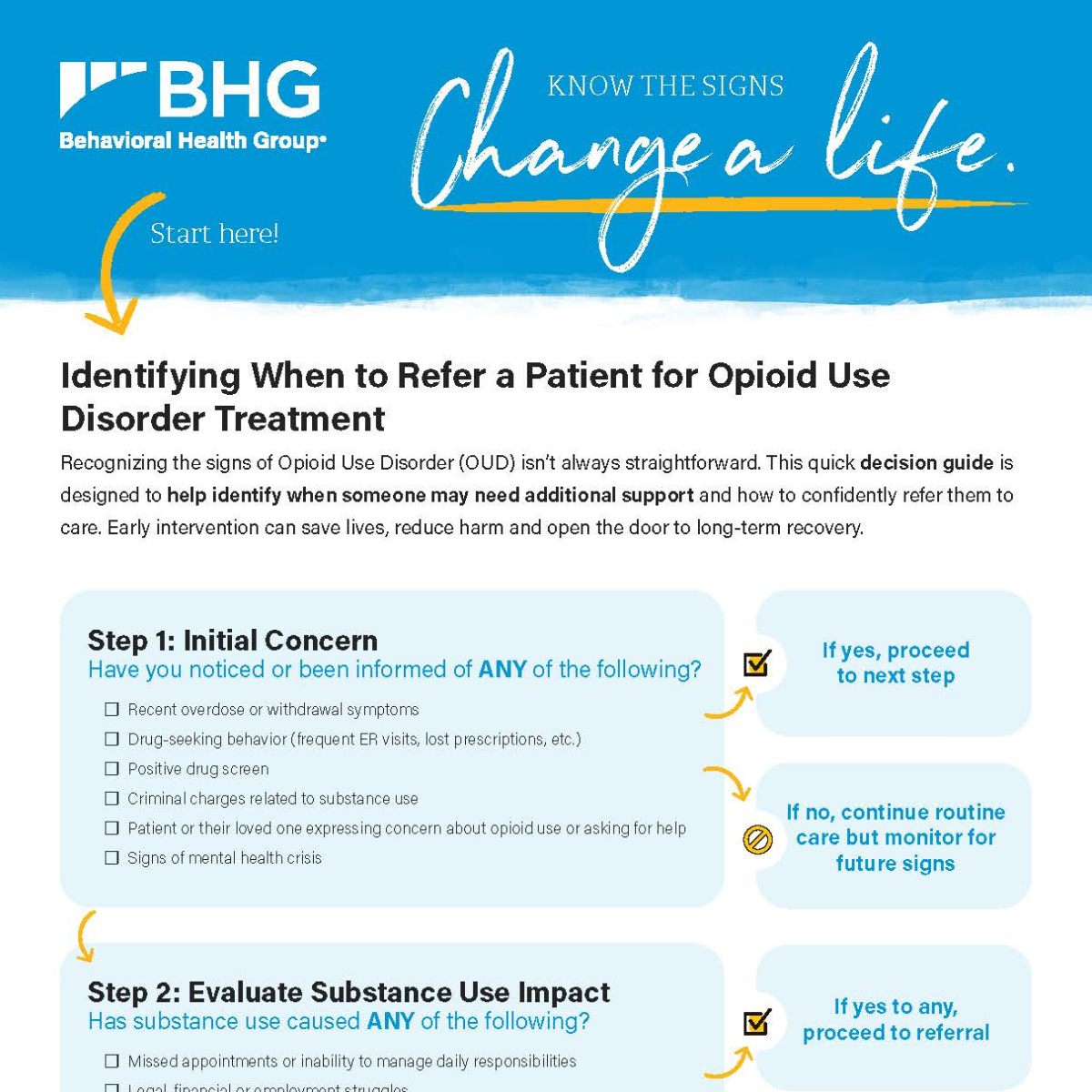
MAT is a comprehensive and evidence-based treatment using a combination of medications and behavioral therapy to treat OUD. The use of medications, also known as medications for opioid use disorder (MOUD), is paired with services that support long-term recovery.
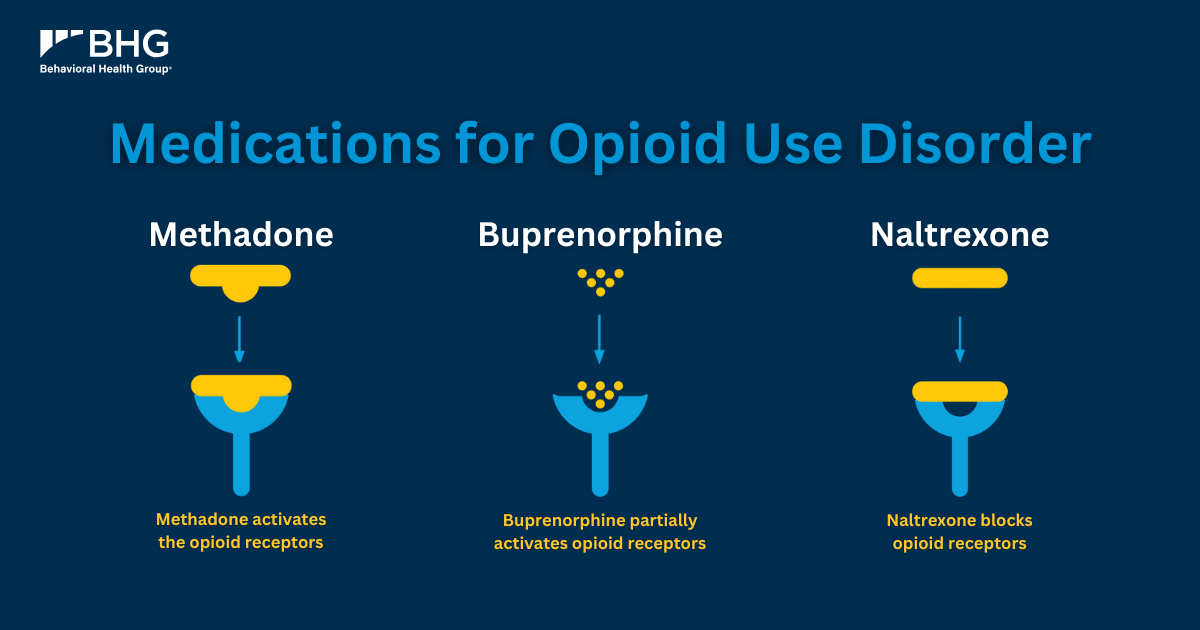
There are three commonly used MOUD: methadone, buprenorphine and naltrexone. Each one works a little differently, but they all help to reduce cravings, block the effects of opioids or ease withdrawal symptoms. These medications are monitored by trained healthcare professionals in settings that prioritize safety and individualized care.
But MAT is more than just medication. Effective treatment also includes wraparound services like individual and group counseling, peer support, case management and other resources that address the mental, emotional and social aspects of recovery. When combined, these services help individuals develop the tools and support networks they need to achieve lasting change.
Common Myths About MAT
Even with growing awareness around OUD and its treatment, there are still many misconceptions around MAT. These myths can create barriers to care, increase ongoing stigma and prevent people from getting the help they need. Let’s take a look at some of the most common myths and the facts to help set the record straight.
Myth 1: MAT is Just Replacing One Addiction with Another
This is something we hear often, and it’s a concern that’s understandable. On the surface, taking medication every day might seem like trading one substance for another. But when we look closer at how MAT works and what addiction really is, it becomes clear that this idea doesn’t reflect the reality of recovery through evidence-based care.
Fact
The confusion comes from not knowing the difference between addiction and physical dependence. Addiction is a chronic health condition that occurs when a person has a hard time stopping their substance use and is often driven by changes in the brain’s reward and control systems. Physical dependence, on the other hand, happens when the body adapts to a substance’s presence that leads to withdrawal symptoms if use stops or is reduced.
MOUD, like methadone and buprenorphine, help stabilize brain chemistry, reduce cravings and prevent withdrawal symptoms, allowing individuals focus on healing, working and reconnecting with their loved ones. These medications are also administered and monitored by providers in safe, structured environments.
In other words, MAT isn’t about swapping one addiction for another. It’s replacing instability with structure, support and a path to recovery.

Myth 2: MAT is Only Meant for Short-Term Use
It’s common to think of treatment as something temporary – something you complete and then move on from. But recovery, especially from OUD, doesn’t follow a one-size-fits-all timeline. The truth is, many people benefit from long-term use of MOUD – and that’s okay.
Fact
Research shows that staying on MAT for an extended period can improve outcomes and reduce the risk of relapse and overdose so there’s no “correct” length of time for MAT. How long MAT should last really depends on individual needs, progress and goals.
Some people choose to leave treatment over time while others continue long-term to maintain stability. Both are valid paths. What matters is that people feel supported and are given the tools they need to stay in recovery.
Myth 3: People Who Use MAT Aren’t Really in Recovery
This myth comes from beliefs about what recovery is supposed to look like. Some assume that “real” recovery means being completely substance-free, including MOUD. But today, most professionals and recovery communities recognize that recovery isn’t about rigid rules – it’s about restoring health, purpose and connection.
Fact
Recovery is a personal process. It’s not defined by abstinence, but by progress – like improved physical and mental health, stronger relationships, and a better quality of life. For many, MAT provides the stability they need to make positive changes and move forward in their lives.
Individuals on MOUD doesn’t mean they’re “less sober” or “not doing the work.” In fact, studies show that people in MAT programs are more likely to stay in treatment, avoid relapse and build healthier, more fulfilling lives.

Myth 4: MAT Should Be a Last Resort
Some people think that medication-assisted treatment is only appropriate after everything else has failed. But this stigma can delay access to life-saving care and put unnecessary pressure on individuals who are ready to begin recovery now.
Fact
MAT isn’t a last resort. It’s evidence-based and is the recommended first line course of treatment for OUD and reduces the risk of overdose. Recovery can begin at any stage and people deserve support whenever they’re ready to seek help. Whether someone is new to treatment or returning after past attempts, what matters most is having access to evidence-based care that meets them where they are. It’s never too late to start treatment. Everyone deserves the chance to recover without having to “hit rock bottom” first.
Myth 5: Methadone Is the Same as Meth
This myth likely stems from the similar-sounding names, but methadone and methamphetamine couldn’t be more different. Confusing the two can create unnecessary fear and stigma around one of the most effective medications used in opioid treatment.
Fact
No, methadone and meth are not the same. Methadoneis a long-acting, FDA-approved medication used to treat OUD. When taken as prescribed, it helps reduce cravings and withdrawal symptoms, allowing people to focus on their recovery. It’s been used safely and effectively for years through certified Opioid Treatment Programs (OTPs).
Methamphetamine, often referred to as meth, is a drug that affects many parts of the body. It’s created in a lab – unrelated to methadone and is not an opioid at all.
The two substances not only have different effects but also serve entirely different purposes. Methadone is a controlled, OUD treatment medication used under medical supervision – nothing like the illegal drug it’s often confused with.
Myth 6: MAT Increases the Risk of Overdose
It’s understandable to have concerns about medications used to treat addiction. But despite this common misconception, the evidence tells a different story.
Fact
MAT does not increase the risk of overdose. In fact, it actually helps reduce the risk. When used as prescribed and under medical supervision, MOUD like methadone and buprenorphine are proven to lower the risk of deadly overdose. They work by stabilizing brain chemistry, reducing cravings and withdrawal symptoms, making it less likely that someone will relapse or use dangerous amounts of opioids again.
Research shows that MAT reduces the likelihood of overdose compared to those who are not in treatment. MOUD are administered with careful dosing and oversight, ensuring they’re used safely and effectively.
Rather than being part of the problem, MAT is one of the strongest tools we have in preventing overdose deaths and supporting long-term recovery.

Myth 7: MAT Medications Are Dangerous
When you really think about it, any medication carries risks, but the idea that medications used in treatment are dangerous is misleading and is deeply rooted in stigma rather than science.
Fact
MOUD, such as methadone, buprenorphine and naltrexone, are all FDA-approved and have been studied for both safety and effectiveness. When prescribed and monitored by a healthcare provider, these medications are safe to use.
Frankly, their safety profiles are comparable to medications used to treat other chronic conditions like diabetes or high blood pressure. Like those medications, MOUD helps people manage a long-term health condition and lead healthier, more stable lives.
What makes these medications safe isn’t just the science; it’s also the structure around their use. They’re prescribed within OTPs designed to monitor dosing, side effects and progress, helping ensure the best possible outcomes for each individual.
The Bottom Line: MAT is a Proven Path to Recovery
MAT is more than just a clinical approach. For many, MAT makes recovery possible and sustainable. It reduces the risk of overdose, supports long-term stability and helps people reconnect with what matters most: health, relationships and a sense of purpose.
It’s time to move past outdated myths and focus on what works. MAT is backed by years of research and supported by leading medical organizations. Most importantly, it helps real people, every day, take back their lives from OUD.
Recovery doesn’t look the same for everyone – and that’s okay. What matters is access to evidence-based care, compassionate support and the opportunity to heal.

MAT with BHG
At Behavioral Health Group (BHG), we understand that recovery is a journey – and no two paths look the same. We offer comprehensive, personalized treatment for OUD that combines FDA-approved MOUD, counseling, case management, peer support and more.
Whether someone is just beginning their recovery or returning to treatment, we meet them where they are with compassion, respect and evidence-based care. If you’re ready to take the next step? We’re here to help. Find a BHG treatment center near you or call 844-535-7291. Referral partners or healthcare providers can call our dedicated referral line at 866-763-2244 or submit an online referral form on our website.